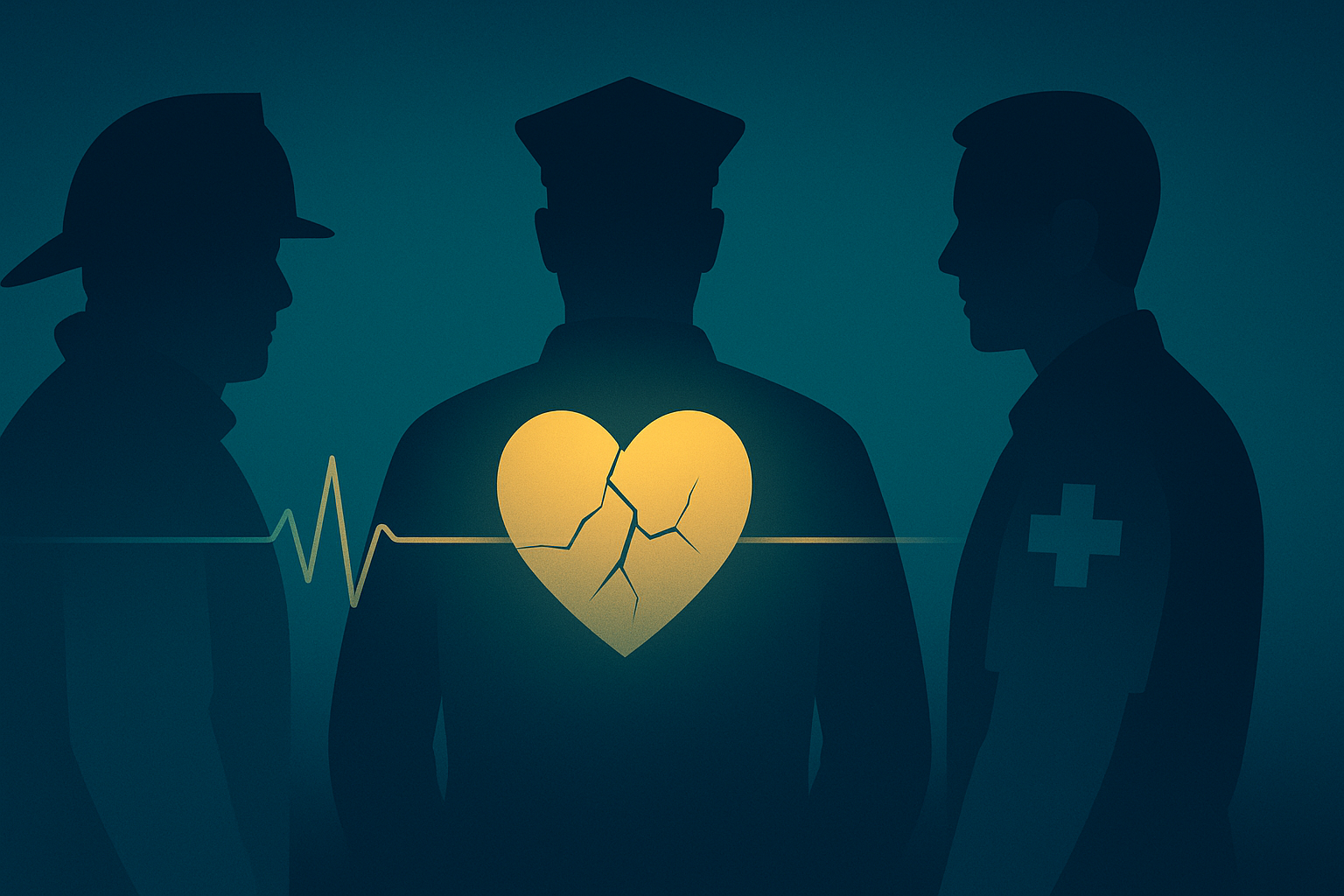
For those on the front lines, trauma doesn't always end when the shift does. Police officers, firefighters, paramedics, and EMTs routinely face situations the average person can barely imagine. Yet, behind the uniforms and stoic expressions, many are silently carrying psychological wounds that never fully heal.
The Weight They Carry
First responders witness death, violence, and human suffering as part of their day-to-day. A 2018 study from the Substance Abuse and Mental Health Services Administration (SAMHSA) ↗ found that an estimated 30% of first responders develop behavioural health conditions, including PTSD, compared to 20% in the general population. Some studies suggest the number may be even higher.
In the UK, Mind reported ↗ that nearly 70% of emergency service workers have experienced a mental health issue due to their work. And yet, stigma, fear of professional consequences, and lack of access prevent many from seeking help.
Stigma, Silence, and Suffering
Despite growing awareness, stigma remains a significant barrier. Research shows that many first responders believe admitting to mental health struggles will make them appear weak or put their careers at risk. This cultural norm of silent suffering runs deep—particularly in environments built on strength, composure, and control.
As a result, mental health support is often delayed until crisis point. And for some, that point comes too late. Suicide rates among first responders are alarming: according to the Ruderman Foundation ↗, more police officers and firefighters die by suicide than in the line of duty in the U.S.
Long Shifts, Delayed Care
Even when help is available, it's often hard to access. NHS waiting times for therapy in the UK can stretch to months. In the U.S., rural areas may have no trauma-informed clinicians within reach. For those working rotating shifts, attending regular therapy can feel impossible.
And yet, the need is urgent. Repeated exposure to trauma—especially without time to decompress or process—is linked to: (1.) Chronic PTSD, (2.) Depression and anxiety, (3.) Sleep disorders, (4.) Substance misuse, (5.) Increased risk of burnout and early retirement.
The Real Cost
Unaddressed PTSD and related conditions don't just harm individuals—they have ripple effects on families, teams, and entire emergency services. The UK College of Paramedics ↗ notes high levels of absenteeism and attrition linked directly to mental health concerns. In the U.S., it's estimated that mental health costs the public safety sector billions each year in turnover, sick days, and disability claims.
"No one who runs towards danger for the rest of us should have to suffer in silence."
A Call for Change
Support must match the sacrifices these workers make. This means: (1.) Trauma-informed care that fits shift-based schedules, (2.) Confidential, stigma-free access to help, (3.) Proactive, not reactive, approaches to mental health, (4.) Scalable solutions that can reach all corners of the service.
At Sentra, we're working to co-develop exactly that with the people who live this reality every day. Because no one who runs towards danger for the rest of us should have to suffer in silence.