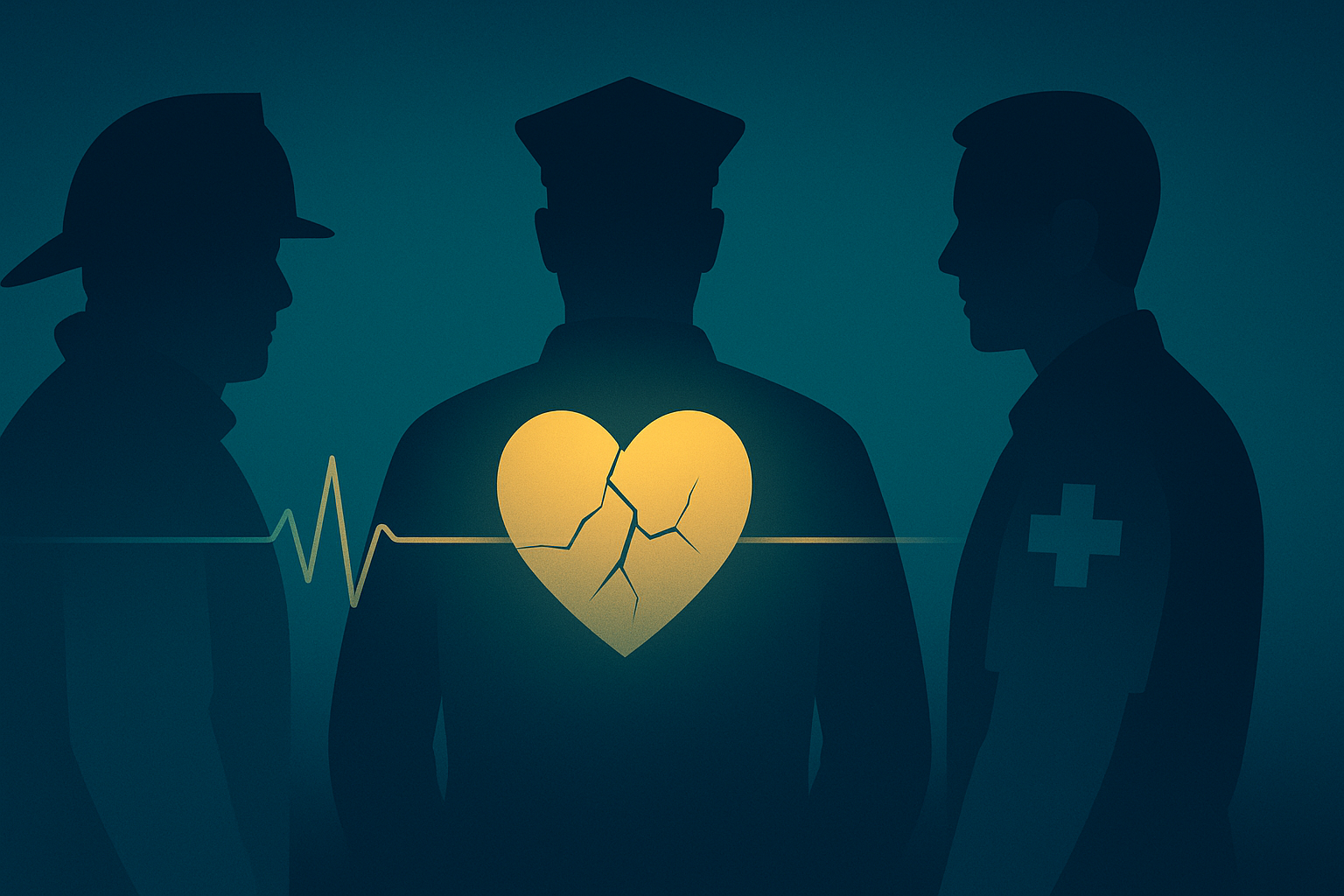
Every May, Mental Health Awareness Week brings colour-themed campaigns and a welcome flood of conversations about anxiety, loneliness and mood. But between the social-media graphics and lunchtime wellbeing sessions there is a group whose struggles rarely trend: the people who run toward danger so the rest of us can walk away.
Police officers and paramedics replay a harrowing call-out on the drive home.
Critical-care nurses can’t remember the last time they slept through the night.
Soldiers keep their war stories locked behind a practised smile.
The data tell a stark story: Veterans—up to 29 % of recent combat veterans will experience post-traumatic stress in their lifetime; First responders—between 7 % and 37 % screen positive for PTSD symptoms; Healthcare workers—49 % of physicians reported burnout in 2024 and one in five felt depressed.
Why the weight is heavier for those who serve
Service cultures prize composure under pressure. That same composure can harden into silence when trauma hits. Shifts are long, rosters unpredictable, and support services often clock off well before the night shift begins. Add the fear of being deemed “unfit for duty”, and many choose to battle on alone—until they no longer can.
The ripple effect at home
Behind every uniform is a family living with the hyper-vigilance, mood swings or emotional withdrawal that trauma can bring. Partners shoulder extra childcare when deployments run long; children learn to read the weather of a parent’s PTSD without having the words for it. Support networks for families remain patchy and under-funded.
When help exists but feels out of reach
Time—appointments that fall in the middle of a 12-hour rota; Access—rural bases or forward deployments where Wi-Fi is a luxury; Stigma—career consequences, real or perceived, for raising a hand; Cost—private therapy can equal a month’s rent.
How Sentra lightens the load
24/7 availability provides support that doesn’t close at 17:00; Trauma-informed pathways offer exercises and check-ins coded from evidence and lived experience; Complete privacy comes from end-to-end encryption and a promise never to sell data; and Collaborative design means veterans, clinicians and first-responders shape every release.
“The bravest thing I ever did was admit I wasn’t OK.”
— Infantry veteran, Sentra beta tester
This week—and every week—reach out
If you are carrying an invisible load, know this: asking for help is serving. Tell a colleague, text a friend, call a helpline in your region (UK: Samaritans 116 123, US: 988). And if you want discreet, always-on support, try Sentra’s live preview and help us build the tool we all wish we’d had.
Service is courage. So is healing. Let’s make room for both.